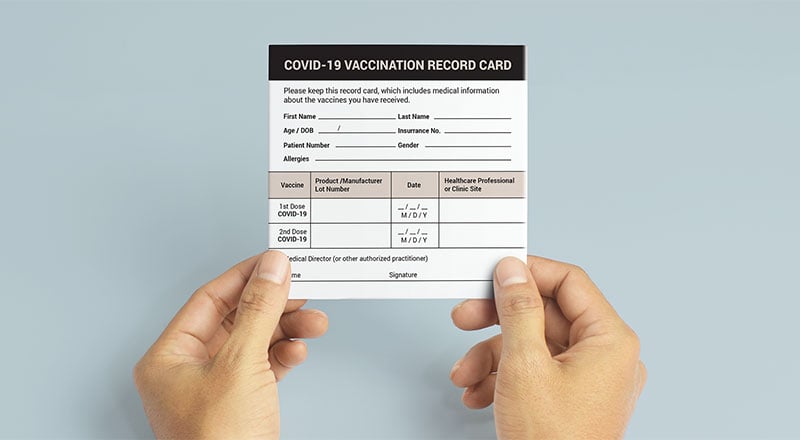
When the results of all these clinical trials are available, a series of steps is required, including reviews of efficacy and safety for regulatory and public health policy approvals. Officials in each country closely review the study data and decide whether to authorize the vaccine for use. A vaccine must be proven to be safe and effective across a broad population before it will be approved and introduced into a national immunization programme. The bar for vaccine safety and efficacy is extremely high, recognizing that vaccines are given to people who are otherwise healthy and specifically free from the illness.
Emerging evidence shows first doses of the vaccine are at least 80 per cent effective at preventing severe illness and longer spacing between doses does not reduce the protection or duration of immunity for multi-dose products. This data include studies in healthcare workers, long term care residents, elderly populations and the general public. Real world vaccine effectiveness is typically lower than what you would see in clinical trials which report 92 per cent protection from symptomatic disease two weeks after a single dose. Third COVID vaccine dose gets green light for some immunocompromised individuals.People whose immune systems are moderately or severely compromised are now encouraged to geta third doseof the Pfizer-BioNTech or Moderna coronavirus vaccine. There isn't yet enough data to evaluate whether an additional dose of the one-shot Johnson & Johnson vaccine is warranted for this limited population, health officials say.
The news impacts the less than 3 percent of American adults whose immune systems are weakened from such conditions as a solid organ transplant or other maladies that have an equally crippling effect on the immune system. These individuals may not have had an adequate immune response from two vaccine doses, and additional doses could help boost protection. Health experts and officials are currently reviewing data to determine if and when booster shots will be needed by the general population. In clinical trials, this vaccine was 66% effective in preventing the COVID-19 virus with symptoms — as of 14 days after vaccination. The vaccine also was 85% effective at preventing severe disease with COVID-19 — at least 28 days after vaccination.
The FDA and the Centers for Disease Control and Prevention have recommended that use of this vaccine continue in the U.S. because the benefits outweigh the risks. If you are given this vaccine, you should be educated about the possible risks and symptoms of a blood clotting problem. In Israel, the early availability of a relatively large per capita vaccine supply made it possible for Israel to give early priority to a large and clearly defined population group – persons over age 60. In doing so, Israel built upon its emergency preparedness, inter-sectoral cooperation, and the organizational and technological capacities of the health plans. Similarly, it required a capacity to rapidly and flexibly mobilize a large number of health care professionals and to set up a sufficient number of sites which were organized for efficient throughput.
The number and geographic distribution of vaccination sites was greatly enhanced by the creative technical response permitting the splitting-up of the large vaccination trays. The panel voted to recommend that adults ages 65 and older and residents of long-term care facilities who received two doses of the Pfizer vaccine should get a booster dose — so should people ages 50 to 64 who have underlying medical conditions. In a separate vote, the committee narrowly agreed that people ages 18 to 49 with underlying medical conditions could also get a booster, depending on their individual risk of getting COVID and the benefit another shot could provide.
The panel then strongly rejected a proposal to allow a booster shot for people whose occupation or institutional setting puts them at high risk for getting or transmitting COVID. This proposal would have provided third shots for health care employees, other front-line workers and people in such institutions as correctional facilities. A growing number of countries across the world are already planning to administer a third dose. The safety level of the vaccine is similar to the safety level of other vaccines. It is safe to assume that the vaccine enhances the effectiveness of the immune response and a higher level of protection is expected with the increase in the number of antibodies. In light of the rising infection rate, a vaccine is the most effective way to fight the coronavirus outbreak.
Generally, these happen shortly after the vaccination and are not associated with more serious or lasting illness. These types of reaction reflect the acute immune response triggered by the body to the vaccines, are typically seen with most types of vaccine and tend to resolve within a day or two. The nature of reported suspected ADRs across all ages is broadly similar, although, as seen in the clinical trials and as is usually seen with other vaccines, they may be reported more frequently in younger adults.
"Our scientific and medical experts conducted an incredibly thorough and thoughtful evaluation of this vaccine. "We have not lost sight that the COVID-19 public health crisis continues in the U.S. and that the public is counting on safe and effective vaccines. The public and medical community can be confident that although we approved this vaccine expeditiously, it was fully in keeping with our existing high standards for vaccines in the U.S." But in a highly unusual move, Walensky overruled the Advisory Committee on Immunization Practices and added approval for people ages 18 to 65 whose job puts them at high risk for contracting or transmitting the coronavirus.
The Pfizer booster will be available to these groups six months after they received their second shot. CDC officials say there is ample supply of the vaccine to provide initial doses to unvaccinated Americans as well as the boosters. In addition, Israel is one of the few countries that have a full population-based childhood immunization registry that includes all of the country's children. Childhood vaccines are provided in Israel free of charge in all well-baby clinics in the country and doses are registered in a web-based registry . Based on the experience from previous mass vaccination campaigns in Israel , the platform of the national registry was quickly adjusted and adapted to the current COVID-19 vaccine campaign.
Notably residents in Israel all have a single unique identifier used in all health care facilities and allowing for ongoing timely data assembly on vaccine doses and number of vaccinees. The registry also allows follow up and assessment of post vaccination adverse events as well as providing real-world vaccine effectiveness data, i.e., "phase 4," or post-marketing, data. However, we do know that there is an increased risk of severe illness requiring hospitalization or ICU care if you get COVID-19 when you are pregnant. In BC and across Canada we prioritize people who are pregnant for early access to vaccines, knowing that this risk can be reduced by protecting people through immunization. So, pregnant people are at increased risk of illness from COVID-19 infection, and can be vaccinated at any time during pregnancy or while breastfeeding.
Do people who are pregnant, trying to get pregnant, or breastfeeding have safety concerns with the vaccine? Getting a COVID-19 vaccine if you are pregnant, planning to get pregnant or breastfeeding is the safest choice to protect you from COVID-19. The Canadian Society of Obstetricians and Gynecologists the National Advisory Committee on Immunization, and public health experts in B.C. All agree that people who are pregnant and breastfeeding should get the vaccine.Evidence about the safety and effectiveness of COVID-19 vaccination during pregnancy has been growing.
Over the last year, while tens of thousands of pregnant and breastfeeding people have been immunized, there has been no increased risk of complications after being immunized. There are no differences in miscarriage, pre-term births, stillbirths or birth defects. And, these real-world study results show that pregnant people have the same, mostly mild, side effects as everyone else. Vaccination and surveillance of large populations means that, by chance, some people will experience and report a new illness or events in the days and weeks after vaccination. A high proportion of people vaccinated early in the vaccination campaign were very elderly, and/or had pre-existing medical conditions. Older age and chronic underlying illnesses make it more likely that coincidental adverse events will occur, especially given the millions of people vaccinated.
It is therefore important that we carefully review these reports to distinguish possible side effects from illness that would have occurred irrespective of vaccination. Fatal cases associated with extremely rare blood clots with lowered platelets are described above. Following vaccination with the mRNA vaccines, people are immune for at least 6 months and likely much longer.
The same is likely to be true for the adenovirus-based vaccines too, but we are still waiting for data. Based on the elements of the immune response activated after vaccination with either the mRNA or adenovirus vaccines, it is likely that immunity will be long-lived. However, decreasing antibody levels in some individuals have prompted a recommendation for some groups of people to get a third dose (See more details in "Why are booster doses being recommended?" question on this page). Also of note, if the virus continues to change, new variants may be able to evade immunity generated by vaccination, which would also affect the duration of protection.
In addition, the vaccination campaign experienced labor pains of its own. During the first few days of the rollout, it was quite difficult to schedule an appointment via the health plans' call centers or digital tools. At some vaccination sites, family of health professionals and members of influential unions or occupations, were vaccinated even though they did not meet the criteria. And, while vaccination sites were set up throughout the country, including in the peripheral regions and in smaller villages and towns, the rate of vaccine uptake was markedly lower than average in Arab localities. In the clinical trials, both mRNA vaccines were about 95 percent effective in preventing COVID-19 after receiving two doses. Protection, beginning 14 days after one dose of either vaccine, is greater than 90 percent.
The duration of protection is not yet known for one or two doses of the vaccine but is being actively monitored. In general, some vaccines provide lifelong immunity, while others such as tetanus only work for 10 years. Indeed, "people resident in facilities are those most at risk for serious forms of the illness and these locations are known to be places where the virus circulates quickly," the health ministry has said. Professionals working in such facilities are therefore particularly exposed. As of January 18, people over 75 who live independently, as well as high-risk individuals under the age of 75, are also eligible for the jab. More than 30.4 million additional doses have been administered worldwide, with many more countries expected to start administering them soon.
Most of the time phase three trials are conducted across multiple countries and multiple sites within a country to assure the findings of the vaccine performance apply to many different populations. All six cases occurred in women between the ages of 18 and 48, six to 13 days after vaccination. People who recently received the Johnson & Johnson vaccine and develop symptoms of severe headache, abdominal pain, leg pain or shortness of breath within three weeks after vaccination should contact their health care provider, officials say. The three vaccines have been found to be highly effective at preventing COVID-19 in clinical trial participants and in real-world data. A large study looking at a diverse population of fully vaccinated health care workers found the two-dose mRNA vaccines from Pfizer-BioNTech and Moderna reduced the risk of getting sick with COVID-19 by 94 percent. In a separate study, researchers found the Pfizer-BioNTech and Moderna vaccines were 94 percent effective against COVID-19 hospitalization among fully vaccinated adults 65 years and older.
Some studies have shown that antibodies were found in the breastmilk of people who received the COVID-19 vaccine which may protect their infant. More studies are needed to determine how much protection this offers. While people who are breastfeeding were not included in most of the vaccine clinical trials, the vaccines are considered safe for people who are breastfeeding because of the way the vaccines work in the body.
Following widespread use of these vaccines across the UK, the vast majority of suspected adverse reaction reports so far confirm the safety profile seen in clinical trials. Most reports relate to injection-site reactions and generalised symptoms such as a 'flu-like' illness, headache, chills, fatigue, nausea, fever, dizziness, weakness, aching muscles, and rapid heartbeat. Generally, these reactions are not associated with more serious illness and likely reflect an expected, normal immune response to the vaccines. Like most vaccines and medicines, clinical trials of COVID-19 vaccine in pregnant women were not carried out prior to use of the vaccines in the general population.
However, evidence from non-clinical studies of the COVID-19 vaccines available in the UK have not raised any concerns about safety in pregnancy. The COVID-19 vaccines do not contain organisms that can multiply in the body, so they cannot infect an unborn baby in the womb. Extensive international experience for the Pfizer/BioNTech Vaccine and COVID-19 Vaccine Moderna used in pregnancy have also not raised any safety concerns. These types of reactions reflect the normal immune response triggered by the body to the vaccines. They are typically seen with most types of vaccine and tend to resolve within a day or two.
The nature of reported suspected side effects is broadly similar across age groups, although, as was seen in clinical trials and as is usually seen with other vaccines, they may be reported more frequently in younger adults. Additional populations may be recommended to receive a booster shot as more data becomes available. The COVID-19 vaccines approved and authorized in the US continue to be effective at reducing risk of severe disease, hospitalization, and death.
Experts are looking at all available data to understand how well the vaccines are working for different populations. This includes looking at how new variants, like Delta, affect vaccine effectiveness. Knowing the potential for a lower immune response, if someone with an immune-compromising condition decides to get vaccinated, it will be important to get both doses and possibly a third dose. They may also choose to practice other public health measures until more is known about their protection against SARS-CoV-2, the virus that causes COVID-19. Some wonder how long they should wait after vaccination before taking these types of medicines, so their immune response is not affected.
Indeed, in the adenovirus vaccine studies, about 1 in 4 vaccine recipients took fever-reducing medication , and most people were still protected from severe disease and all were protected against hospitalization. This is achieved by generating immune memory cells, such as B cells and T cells. These cells are typically long-lived and reside in the bone marrow, bloodstream, and lymph glands to monitor for exposure to a pathogen. If the pathogen is detected, these memory cells quickly become activated and stimulate the immune response to efficiently fight the infection before the infection can get out of control and cause serious illness. Data shows that any of the currently authorized COVID-19 vaccines can be offered to people who are pregnant or breastfeeding. Pregnant people are at increased risk for severe illness from COVID-19, which could result in intensive care admission, mechanical ventilation or even death.
In addition, pregnant people with COVID might be at increased risk of adverse pregnancy outcomes, such as preterm birth, compared with pregnant women without COVID-19. Getting vaccinated is a personal choice, so if you have any questions, a conversation with your health provider might help. In the clinical trials, the AstraZeneca COVID-19 vaccine was about 62% effective in preventing symptomatic disease starting 2 weeks after the second dose. However, AstraZeneca confirms 100% protection against severe disease, hospitalization and death in the primary analysis of their Phase III trials. No adverse side effects were reported in pregnant women who took part in the clinical trials, be it with regard to the pregnancy itself or in the development of the foetus during the preclinical trials led by Pfizer and Moderna on animals.
However, pregnant women are currently excluded from the vaccination campaign while targeted studies are conducted. According to the European Medicines Agency, vaccination will only be considered once the expected benefit exceeds the potential risk. As far as breastfeeding is concerned, there is not yet data on the vaccine's potential to transfer into breastmilk after the mother is inoculated. Fully vaccinated people who get a breakthrough coronavirus infection are about half as likely to experience persisting symptoms of COVID-19, known as long COVID, compared to unvaccinated people who get infected with the virus, a new study shows. The report, published in The Lancet Infectious Diseases, is based on data from the COVID Symptom Study app. It found that fully vaccinated adults who had a breakthrough infection were 49 percent less likely to have symptoms lasting at least four weeks after infection.
Long COVID has affected millions of people since the start of the pandemic, and many have reported debilitating symptoms. As a result, clinics have popped up all over the country to study the phenomenon and to help these so-called long-haulers get back to normal. A second shot of the Johnson & Johnson COVID-19 vaccine will increase protection against symptoms and severe disease, according to the drug company. J&J has so far been a single-dose vaccine and the manufacturer's booster data has not yet been peer reviewed. The company says its COVID-19 booster shot is 94 percent effective when given two months after the first dose and that the additional shot also increases antibody levels by four to six times compared with the one-dose regimen.
Company officials also say they have submitted their data to the FDA, which would have to approve the use of a second J&J shot. Moderna has asked the FDA to consider authorizing a booster dose of its vaccine; the FDA on Sept. 22 amended Pfizer's authorization to include boosters for some Americans. As we receive more reports of these types of reactions with more exposure to the COVID-19 vaccines, we are building a picture of how individuals are experiencing them and the different ways that side effects may present in people. Similar to the flu like illness reported in clinical trials, these effects may last a day or two. The Pfizer/BioNTech jab is one of two mRNA vaccines along with Moderna's and it was found to be 95 percent effective in Phase III trials.
Israel's real world experience with the shot has closely replicated those results after the government obtained large quantities of the vaccine in exchange for sharing information on its effectiveness. Clalit Health Services, the country's largest healthcare provider, has released the results of a study of more than half a million fully vaccinated Israelis which indicates the Pfizer/BioNTech shot provides 94 percent protection. The evidence has shown high levels of short-term protection from the first dose of the Pfizer-BioNTech vaccine, the AstraZeneca vaccine and the Moderna vaccine, including against severe disease. The second dose is important to provide longer lasting protection and is expected to be as or more effective when given at an interval of 8 weeks from the first dose. Whether or not diagnosed with coeliac disease, people who have had an allergic reaction to a previous dose of COVID-19 vaccine, or a component of the COVID-19 vaccine should not be given the vaccination. Anyone due to receive their vaccine should continue with their appointment and discuss any questions, serious allergies or any other medical conditions with the healthcare professional before having the vaccine.
When a high proportion of a population receive an effective vaccine it becomes difficult for the disease to spread. This gives protection to vulnerable people such as newborn babies and other people who can't be vaccinated, which is known as herd immunity. It is not clear what proportion of people would be required to be vaccinated to achieve this because the vaccines against the disease are new and COVID-19 is a global pandemic infection. Therefore, the best protection you can have is to have the vaccination when you are invited to attend and to continue to follow measures to reduce spread like social distancing, hand and respiratory hygiene and face coverings where advised. FDA-approved vaccines undergo the agency's standard process for reviewing the quality, safety and effectiveness of medical products. For all vaccines, the FDA evaluates data and information included in the manufacturer's submission of a biologics license application .
A BLA is a comprehensive document that is submitted to the agency providing very specific requirements. The agency conducts its own analyses of the information in the BLA to make sure the vaccine is safe and effective and meets the FDA's standards for approval. In early February, company officials announced that phase 3 clinical trial results showed that their vaccine was 82 percent effective after 12 weeks.

























No comments:
Post a Comment
Note: Only a member of this blog may post a comment.